Lilly gets FDA OK of modified dosing for Alzheimer’s drug
Dive Brief:
- The Food and Drug Administration has approved a modified dosing schedule for Eli Lilly’s Alzheimer’s disease drug Kisunla, permitting a smaller first dose and a more gradual increase that in clinical trials, reduced dangerous episodes of brain swelling, the company said Tuesday.
- That side effect, called ARIA, has made physicians reluctant to prescribe the drug and resulted in its use being blocked in some countries. The new dosing protocol will “aid healthcare professionals in evaluating appropriate treatment options for their patients,” said Brandy Matthews, Lilly’s vice president for Alzheimer’s medical affairs, in a statement.
- Approved in 2024, Kisunla was the third drug cleared by the FDA to slow Alzheimer’s progression by targeting toxic plaques of a protein called amyloid beta. Despite its potency, sales were only a modest $21 million in the first quarter of 2025.
Dive Insight:
The new dosing protocol recommends physicians give patients a single 350 milligram vial of Kisunla for their first monthly intravenous infusion, rather than two vials, and then three vials rather than two for their third dose two months later. On their fourth and subsequent doses, patients will receive four vials.
The recommendations was based on the results of the Trailblazer-Alz 6 study, which found a statistically significant difference in ARIA episodes through 24 weeks of treatment between those who got the modified dosing and those who got the originally approved dosage, 14% versus 24%.
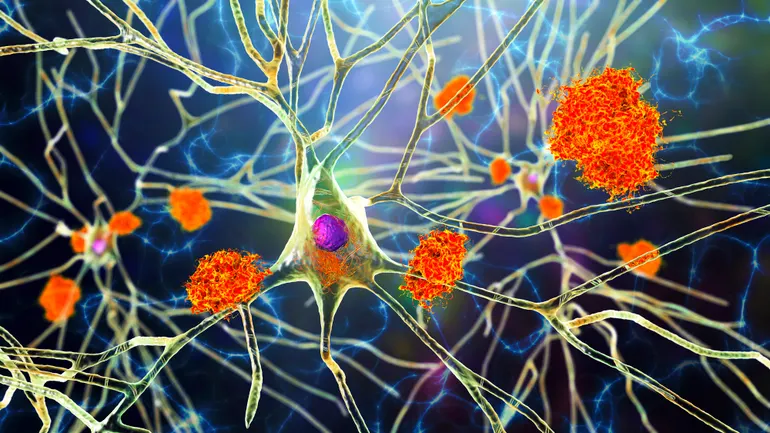
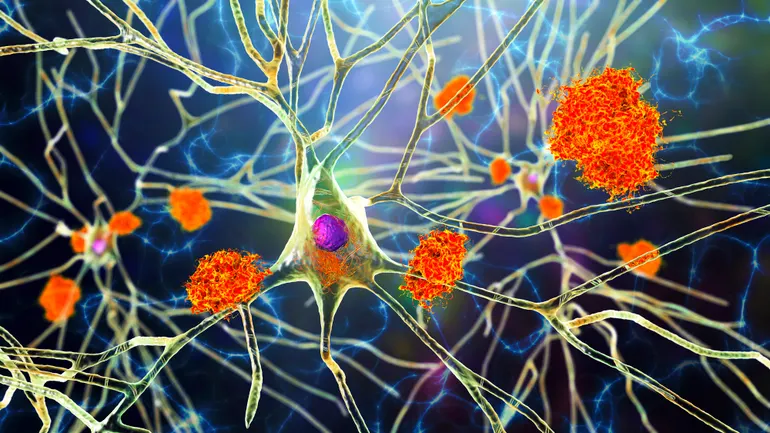
Kisunla is one of only two disease-modifying Alzheimer’s disease drugs on the market, along with Eisai and Biogen’s Leqembi, both of which treat the disorder by binding to and removing amyloid beta from the brain. Deposits of amyloid are a characteristic of Alzheimer’s and are believed to disrupt and kill nerve cells in the brain. (A third drug, Biogen’s Aduhelm, was effectively withdrawn.)
Kisunla was effective enough in removing brain amyloid that 72% of trial participants receiving it in a clinical trial stopped taking it after 18 months.
However, ARIA is a side effect of both drugs, and Kisunla is associated with higher rates of ARIA than Leqembi. Many physicians and patients have judged the risk greater than the benefit, which is about a half year of delayed progression.
The risk-benefit debate has caused a regulatory split, as outside advisers to the FDA unanimously supported its approval ahead of the final decision, while European regulators said no. And while the U.K. has licensed the drug for use, its cost-effectiveness agency has said its modest benefit doesn’t justify its price, which in the U.S. is $32,000 a year. (The UK price is still listed as “confidential” in agency documents.)
Kisunla has also been approved in Japan.
This post has been syndicated from a third-party source. View the original article here.




