Medicare will negotiate Novo’s GLP-1 drug price. Here’s what that means for Ozempic, Wegovy.
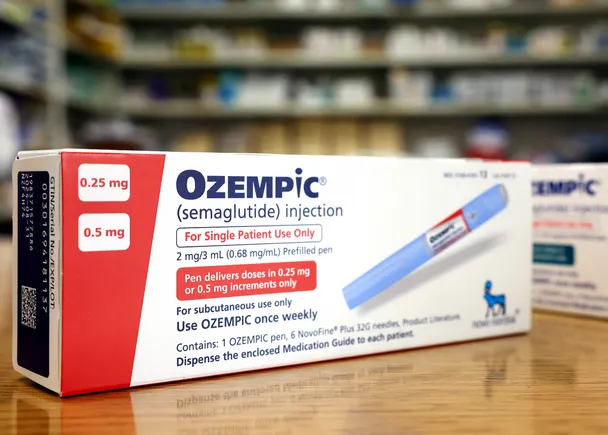
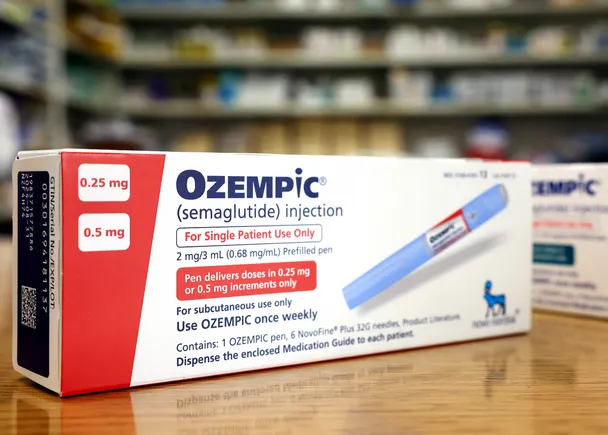
Medicare’s next drug price negotiations will treat Novo Nordisk’s semaglutide as a single product, regardless of whether the metabolic disease medicine is used to treat diabetes or heart risk, and whether it is delivered by shot or pill.
Semaglutide was one of 15 drugs the Centers for Medicare and Medicaid Services selected Friday for a second round of price talks set up by the Inflation Reduction Act. Besides semaglutide, which Novo Nordisk sells as Ozempic, Rybelsus and Wegovy, the agency also chose other diabetes drugs, respiratory therapies and several cancer treatments.
CMS’ treatment of semaglutide as one product is because the agency focuses on a drug’s “active moiety,” or the core compound that has a biological effect, rather than treat each use approved by the Food and Drug Administration separately.
“The statute and our guidance [are] very clear that when a drug is selected for negotiation, all dosage forms and strengths with the same active ingredients are included, even if they are sold under different formulations or brand names,” said Erin Richardson, CMS’ chief of staff, on a call with reporters.
Ozempic was approved in 2017, making semaglutide subject to negotiation for the first time in 2025 under rules laid out in the Inflation Reduction Act. Eli Lilly’s competing products Mounjaro and Zepbound, which contain the active ingredient tirzepatide, gained first approval in 2022, meaning they wouldn’t be subject to price negotiation until 2030.
While semaglutide is widely covered within Medicare for diabetes, the health insurance program is not currently permitted by law to reimburse for treating weight loss, where Novo has since 2021 sold semaglutide as Wegovy.
Wegovy is also approved to lower cardiovascular risk in people with heart disease and who are either overweight or have obesity, however. Medicare determined last March that this use could be covered under Part D plans. And the Biden administration last fall proposed a new rule permitting Medicare to cover obesity treatment more broadly.
The “maximum fair price” the U.S. government negotiates under these talks will be a single cost. Dosage strengths, formulations and packaging prices for Ozempic, Rybelsus and Wegovy would be adjusted to meet that monthly price.
Semaglutide products in Medicare are also already likely to be discounted from their list prices — $998 a month for Ozempic and Rybelsus, $1,349 a month for Wegovy — although CMS officials wouldn’t confirm that Part D insurance plans receive rebates. In 2023, Novo paid 62% of its gross sales back in rebates across its sales. Of roughly $88.3 billion in gross sales, about $32 billion was paid back in rebates to Medicare and U.S. managed care plans.
“We remain committed to working with policymakers to advance solutions to ensure access and affordability for all patients,” a Novo spokesperson said in an emailed statement. “That is why we are deeply concerned about the price-setting process, which could negatively impact patients’ ability to access their medicines and threatens to stifle future scientific development of life-changing medicines for chronic diseases in which there is a real unmet need.”
Negotiations over semaglutide will be Novo’s second time discussing price concessions with CMS. The first round of talks, which yielded prices set to take effect in 2026, included insulin aspart, which Novo sells as several different products.
That selection triggered a lawsuit from Novo, citing CMS inclusion of multiple products by way of selecting one active ingredient.
That suit could provide an opportunity, albeit a long shot, to exempt Wegovy and Rybelsus from this round of price negotiations. CMS in its guidance said it applies price negotiations across products using the same active ingredient or moiety because it reduces the incentive for companies to engage in “product hopping,” or making small changes in drug formulation to extend patent-protected exclusivity.
Novo claimed the guidance went beyond what the IRA allowed because it interpreted the law’s call for price negotiations on “drug products” and “biological products” to mean all those with the same active moiety or ingredient. By grouping together all of Novo’s insulin products, CMS invoked negotiations on more than the 10 products permitted by the IRA in the initial round, Novo argued.
The courts so far have rejected Novo’s lawsuit, ruling in July the company was effectively suing on behalf of other manufacturers when it made that claim, which it doesn’t have standing to do. Novo has appealed.
Whether CMS will be able to carry out its plans — and even whether the program will survive a Trump administration and Republican Congress seeking to undo the work of the Biden administration — is subject to some question. Already, drugmakers are reportedly planning to ask the Trump administration to pause negotiations.
On the call with reporters, CMS officials emphasized their selections were guided by the Inflation Reduction act, noting that any other team that followed statute would end up choosing the same slate of 15 medicines.
This post has been syndicated from a third-party source. View the original article here.